(adapted from TFPC, 1997)
Although we have no current estimates, and despite what we know about the food-health connection, food as health promotion receives only a very small percentage of total health care spending, certainly less than 0.1%.
Given the current financial pressures on the health care system, and assuming that no additional resources will be devoted to it overall, then getting started will require the reallocation of money from other places in the system. Enormous savings are to be had, but unfortunately, because of the current structure of health care delivery, a reduction in the demands for services will not necessarily translate into savings to transfer to another area. This occurs for three reasons: a) because demand for many health services is elastic since hospitals and physicians "create" new demand for their services; b) because so much has already been invested in overcapacity (e.g., buildings, high-technology equipment, and specialists); and c) because there is little budgetary connection between different components of the system (e.g., an individual hospital budget and the neighbourhood CHC) (Rachlis and Kushner, 1994).
There appear to be three main ways to jumpstart the financing transition:
1. Provincial regulation is needed to ensure that large institution and collective physician budgets are reduced and those dollars reallocated to other priorities. Most provinces have been attempting to do part of this through their (often difficult) negotiations with medical and hospital associations over fee schedules and allocations, but this effort has largely been in the service of curtailing budgets as opposed to reallocation to prevention. Much of the debate is over the administration of health care and the size of allocations, as opposed to putting in place the measures that will create a healthier population that has less need of health care services.
The Windsor District Health Council (DHC) from the mid-1990s provided a possible model for future reallocations. That DHC made an agreement with the NDP provincial government of the day (rescinded by the subsequent PC administration) to save money through hospital amalgamations, and retain the savings within the Windsor health area. The DHC oversaw the reduction of hospitals from 4 to 2 and then invested many of the savings in community-based primary care and health promotion programs. This was only possible because the provincial government provided oversight and regulated the reallocation of the savings from the hospital sector to the community one. Unfortunately, with the change of government the agreement and associated regulations were eliminated, so the implications of this approach are not well understood.
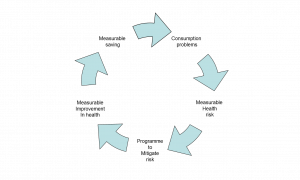
2. The same kind of thinking can be used at a food programme level to capture savings. In the idealized programme delivery cycle (see figure below), a food consumption problem generates a measurable health risk that is addressed with a specific program design to mitigate the risk. The programme is effective and reduces the health risk and the incidence of morbidity and mortality, which reduces the demand for acute health care services and generates savings. In theory, the savings can then be reinvested in a new cycle. It has been known for years that even very conservative program designs with a narrow view of the food-health relationship can generate $2-3 in savings for every $1 invested (TFPC, 1997). Wider angle health promotion initiatives are thought to return $4-5 in savings for every $1 (Aldana, 2001). But because these savings occur in other parts of the health care system, they are not credited to the food programming and are not reinvested in more programming that is effective. Equally problematic, many food interventions have a more diffused and less measurable impact on health, or the impact occurs over a very long time horizon (see discussion about compression of morbidity).
As discussed in the transition stages, the provinces will have to mandate the delivery of certain kinds of food programs with relatively definitive evidence at various sites across the health care system, including primary care teams, public health units, CHCs, and hospitals. These programs could be directly funded by the province, they could be part of fee payment incentive structures as currently happens on a limited basis for some primary care teams, and they could be part of mandatory core public health programming. They have to be mandatory and funded by the province because the savings are system-wide and cannot be targeted to specific kinds of reinvestments by using regulatory measures, as in scenario 1.
3. Use the Federal-Provincial Health Accord process to allocate monies for the transition that can be recouped later. The recent (2017) province by province negotiations over health care funding revealed that it is possible once again for the federal government to use its funding authority to press the provinces to improve programming in specific areas, in this last cycle mental health and home care. Food and other health promotion measures could be the focus of the next Health Accord cycle. Giving it a high priority is a challenge, given all the difficulties the health care system is facing, but if Health Accord negotiations stay on a 10-year cycle, and many efficiency and substitution strategies are underway, food could feasibly rise much higher on the health care agenda.
Not to be discounted is the potential for shifts to an optimal diet to create new economic activity and employment. This has not been well studied in Canada, particularly for the transition strategies proposed here. But Mukhopadhyay and Thomassin (2012) used the federal government's input-output models to estimate the economic impacts of a population-wide shift to a diet based on the 2007 version of the Canada Food Guide. This version of the Guide is far from an optimal diet scenario, and the 2018 version of the Guide encourages more shifts than the early version, so their modelling is decidedly conservative relative to what is proposed on this site. However, they found that the net impacts of such dietary shifts to increase fruit, vegetable, dairy and grain consumption, with less meat, had positive impacts on employment and GDP. Obviously, the meat sectors, and up and downstream industries, would be negatively affected, but the advantages associated with growth in the other production areas would exceed those negative impacts. Such positive economic effects create the possibility of additional transition financing from general tax revenue increases associated with these increases.